(HealthDay News) — (Tasrir) — Alzheimer’s disease is the most common type of dementia. Here, we break down what to know about this disease, including:
-
What Alzheimer’s disease is
-
The difference between Alzheimer’s and dementia
-
The causes of Alzheimer’s disease
-
Alzheimer’s disease symptoms
-
The stages of Alzheimer’s
-
Alzheimer’s disease treatments
-
How to prevent Alzheimer’s disease
-
What living with Alzheimer’s disease is like
What is Alzheimer’s?
Symptoms grow worse over time and may interfere with a person’s ability to perform everyday tasks because their thinking and processing patterns change.
Because Alzheimer’s starts in the part of the brain that affects learning, the first signs are often changes in memory, and exhibiting poor thinking and reasoning skills. As the disease progresses, you will notice changes in behavior and the person becoming confused.
Most people with Alzheimer’s are 65 or older, according to the Alzheimer’s Association, but it may affect younger people as well. Younger people with Alzheimer’s are said to have early-onset Alzheimer’s disease.
Although Alzheimer’s disease largely affects older people, it’s not the result of aging.
Alzheimer’s is the most common type of dementia, the general term for a decline in memory, reasoning and thinking skills. As many as 60% to 80% of dementia cases are Alzheimer’s, notes the Alzheimer’s Association. However, not all dementia is Alzheimer’s.
Alzheimer’s vs. dementia: What’s the difference?
Dementia is a catchall phrase for a number of disorders that affect the brain and behavior. To be called dementia, the loss of memory and thinking skills have to be severe enough to make daily living challenging. Dementia is more than the mild forgetfulness that often comes with aging.
Alzheimer’s is one type of dementia. In other words, Alzheimer’s is dementia, but not all dementia is Alzheimer’s. Other types of dementia include vascular, Lewy body, frontotemporal dementia and mixed dementia. Of the different types, Alzheimer’s is the most common.
Other diseases that may cause dementia include:
-
Limbic-predominant age-related TDP-43 encephalopathy
-
Chronic traumatic encephalopathy
-
Parkinson’s disease dementia
-
Creutzfeldt-Jakob disease
-
Huntington’s disease
Researchers do not know what causes some people to develop Alzheimer’s. A combination of things are believed to play a role. These include age-related changes in the brain, along with a person’s genes, environment and lifestyle. How much each factor matters can vary from person to person.
In general, scientists are looking at age-related factors in the brain, such as:
-
Shrinking
-
Inflammation
-
Vascular damage
-
Free radicals (unstable molecules that cause cell damage)
-
Loss of energy production in brain cells
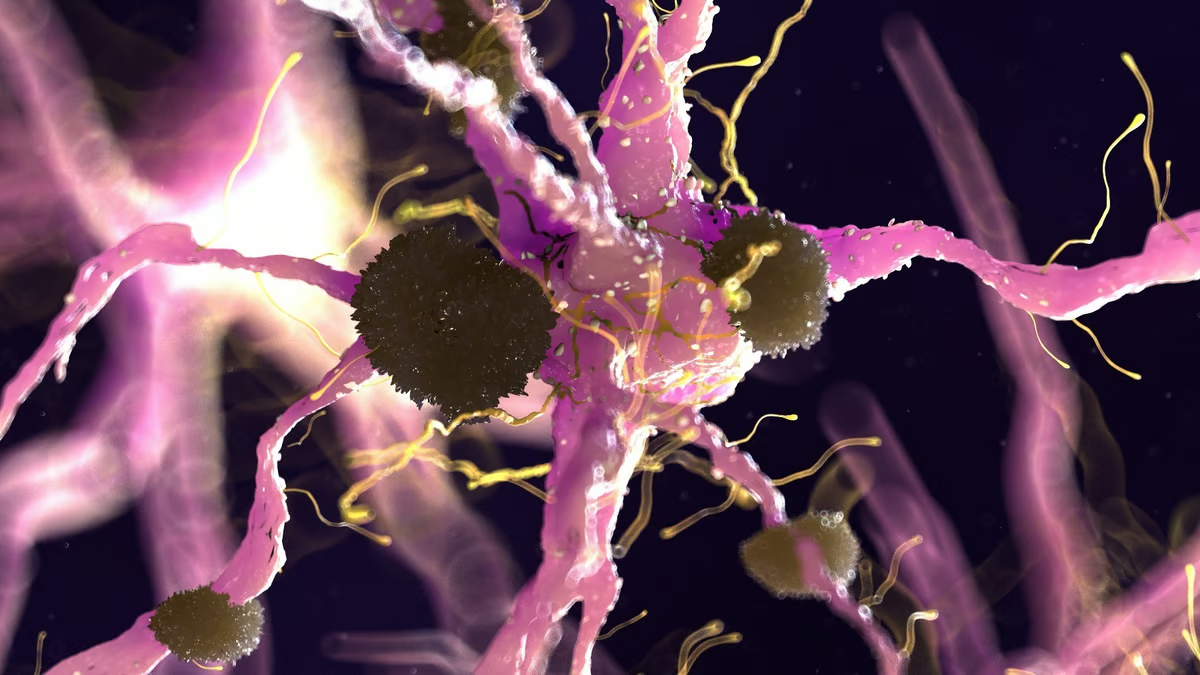
The brain is made up of tens of billions of cells called neurons. Neurons process and transmit information from the brain to muscles and organs. Alzheimer’s results when this communication among neurons is disrupted. When neurons are damaged, they lose their connections to one another and eventually die.
Much of the research on the cause of Alzheimer’s is focused on two cell proteins: beta amyloid and tau.
-
Beta amyloid, a protein fragment, may clump together with other cell debris and form deposits called amyloid plaques. When they do, they may have a toxic effect on neurons and disrupt their ability to communicate with other brain cells.
-
Tau proteins provide internal support and carry nutrients and other essentials. In the brains of people with Alzheimer’s, tau proteins change shape and form structures called neurofibrillary tangles. Like plaques, tangles disrupt the brain cell transport system and damage cells.
Is Alzheimer’s genetic?
If you have a parent or sibling that has been diagnosed with Alzheimer’s, you have a slightly higher risk for the disease as well. However, genetic factors that affect Alzheimer’s are not completely understood.
One gene, apolipoprotein E (APOE) is believed to increase the risk of developing Alzheimer’s. However, not everyone with this gene will. About 25% to 30% of the world’s population carry this gene, according to Mayo Clinic.
Research has shown that rare changes in three genes pretty much guarantees that people who inherit them will develop Alzheimer’s, according to Mayo Clinic. However, these changes have been seen in less than 1% of people with Alzheimer’s.
Other risk factors for Alzheimer’s
Some other risk factors for Alzheimer’s include the following.
Sex: More women than men develop Alzheimer’s. However, it may be because women live longer.
Mild cognitive impairment (MCI): The risk of developing Alzheimer’s is higher in people with MCI. This is particularly true for people whose MCI affects mainly their memory. Their disease is more likely to progress to Alzheimer’s.
Head trauma: People 50 years of age and older who suffer a traumatic brain injury (TBI) are at an increased risk for dementia and Alzheimer’s. The more severe the head trauma, the greater the risk. The same is true for people who suffer multiple head injuries. The risk may peak within the first 2 months to 2 years of suffering a head injury.
Air pollution: Some animal research has linked exposure to air pollutants such as traffic exhaust and burning wood to the risk of dementia, but more research is needed.
Alcohol consumption: Drinking excessive amounts of alcohol may cause brain changes. These brain changes may increase the risk for dementia, particularly early-onset dementia.
Sleep patterns: People who sleep poorly may have an increased risk of Alzheimer’s. This may include trouble falling asleep or staying asleep.
Heart health: Some of the risk factors associated with heart disease may also be the same for Alzheimer’s. These risk factors include:
-
Living a sedentary lifestyle
-
Being obese
-
Smoking or exposure to secondhand smoke
-
Having high blood pressure
-
Having high cholesterol
-
Not controlling type 2 diabetes well
Socializing: Research has shown that people who don’t stimulate their brains or engage with others are more likely to develop Alzheimer’s.
Memory loss that is more than normal aging is often the first sign of Alzheimer’s. People may have trouble remembering everyday things and cannot think clearly. Other symptoms may include:
-
Repeating questions and statements over and over
-
Forgetting appointments and other events
-
Putting items in places they don’t belong
-
Getting lost in familiar places
-
Forgetting the names of people and things
-
Having trouble finding the right words to express themselves and to contribute to conversations
Trouble with numbers
People with Alzheimer’s often have trouble with numbers. They find it difficult to balance their checking accounts and to pay bills by their due date. Eventually, they may not be able to do even simple math or recognize numbers.
Decision-making
As Alzheimer’s progresses, people with the disease may make poor choices, such as wearing shorts and a T-shirt on a cold winter day. They may leave food to burn on the stove, or get lost when driving to places they have driven to numerous times in their past.
Personality changes
The part of the brain that affects mood and behavior is also affected. As a result, people with Alzheimer’s may often:
-
Become depressed
-
Lose interest in activities they might have previously enjoyed
-
Withdraw from social activities
-
Become angry or aggressive
-
Wander aimlessly
-
Lose any social inhibitions
-
Are delusional, such as thinking that something has been stolen or taken from them when it was not
People with Alzheimer’s disease may still be able to read, listen to books, sing, enjoy listening to music, dance and do crafts, as well as other things.
Alzheimer’s disease is progressive, meaning it gets worse with time. The disease is divided into stages, with each having its own symptoms. Here are the 7 stages:
Stage 1: No dementia seen
People appear to have normal mental health and don’t have signs of decline. Changes in the brain have started, but there are no outward symptoms yet.
Stage 2: Some memory loss and age-related dementia
People can’t recall names or other things that they used to be able to do. Many chalk it up to growing older. This stage may last 15 years or so.
Stage 3: Mild Alzheimer’s disease
In this stage, you might notice that the person:
-
Gets lost in familiar places
-
Can’t handle money or pay bills
-
Repeats the same questions no matter how often you give the same answer
-
Takes longer to get dressed and eat, as well as do other daily tasks
-
Exhibits some personality and behavioral changes
People are often diagnosed when they are in this stage.
Stage 4: Moderate Alzheimer’s disease
Memory loss and confusion worsens. People with this stage of the disease may no longer be able to recognize family members and friends. They can’t learn how to do new things or execute tasks that require a number of steps, such as getting dressed. They may also:
-
Behave impulsively
-
Have hallucinations and delusions
-
Become paranoid
They deny they have Alzheimer’s as a coping mechanism.
Stage 5: Moderately severe decline
People have trouble with everyday tasks. They may wear the same clothing day after day and don’t dress appropriately for the summer heat or winter cold. They withdraw from activities with family and friends.
Stage 6: Moderately severe dementia and cognitive decline
This stage lasts about 2.5 years and makes it difficult for the person to live independently. They can’t dress or bathe themselves. They confuse people they have long known, such as a spouse or child. They can’t recall the events of their day when asked.
Stage 7: Very severe cognitive decline and severe dementia
At this stage, the person requires full-time help with daily living tasks, such as dressing and eating. They can no longer communicate with others. They may be bed-ridden.
Alzheimer’s medications
There is no cure for Alzheimer’s disease at this point. However, new drugs are in development that show promise. Research is targeting underlying causes and may provide ways of stabilizing memory and thinking skills. Two drugs have been approved by the U.S. Food and Drug Administration (FDA) to change the progression of the disease:
-
Lecanemab (Leqembi®): This drug has shown to slow the progression of the disease in some people. It may be given to people with early onset disease who show high levels of beta-amyloid in the brain. It is given as an infusion every two weeks. Common side effects include infusion-related reactions, temporary swelling of the brain and headache.
-
Aducanumab (Aduhelm®): This drug is given as an infusion every month. It is used to treat early Alzheimer’s disease, including those with mild dementia. Common side effects include temporary swelling of the brain, headache and falls.
Drugs that treat cognitive symptoms of Alzheimer’s include:
Cholinesterase inhibitors, which treat memory, thinking, language, judgment and other thought processes:
-
Donepezil (Aricept®): It has been approved to treat all stages of the disease.
-
Rivastigmine (Exelon®): It has been approved for mild-to-moderate Alzheimer’s and for mild-to-moderate dementia that is associated with Parkinson’s disease.
-
Galantamine (Razadyne®): It has been approved for mild-to-moderate stages of Alzheimer’s disease.
Glutamate regulators, which help improve memory, attention, reasoning ability, language and the ability to perform daily tasks.
-
Memantine (Namenda®): It has been approved for moderate-to-severe Alzheimer’s disease.
A combination drug with donepezil and memantine (Namzaric®) is a cholinesterase inhibitor and a glutamate regulator. It has been approved for moderate-to-severe Alzheimer’s disease.
These drugs have possible side effects, including:
-
Nausea
-
Vomiting
-
Loss of appetite
-
Muscle cramps
-
Increased frequency of bowel movements
-
Dizziness
Additional treatments
Healthcare providers may also treat other conditions that travel with Alzheimer’s, such as:
-
Sleeplessness
-
Agitation
-
Other symptoms that affect behavior and mental health
Patients with these related conditions may be given drugs to treat insomnia, antidepressants, anti-anxiety drugs or antipsychotics if other lifestyle, stress-reduction and supportive treatments don’t seem to be working.
As of now, Alzheimer’s disease is not preventable. However, some things may lower your risk for developing Alzheimer’s and staying sharp. It’s the focus of much research, so our understanding will only improve more and more over time.
Here are some things you may do.
A number of studies have shown that exercise may reduce the risk of developing Alzheimer’s as people age. Aim for a minimum of 150 minutes of moderate-intensity exercise weekly, which is noted by many health experts, including Alzheimer’s.gov, as a baseline for good health.
Eat well
Following a nutritious diet is important to help stave off a number of conditions, such as high blood pressure. Add dementia to that list. The Mediterranean diet, which emphasizes fruits, vegetables, whole grains, legumes, fish and other seafood, and unsaturated fats such as olive oil, shows promise in warding off Alzheimer’s, according to the National Institute on Aging. So does the MIND diet, which focuses on plant-based foods.
Both the Mediterranean and MIND diets limit the amount of red meat, sweets, butter/margarine and fast foods.
Keep a healthy weight
People who are overweight or obese are at increased risk for not only diabetes and heart disease, but also dementia and Alzheimer’s. Being physically active and choosing a healthy diet may help to maintain a weight that’s healthy for you.
According to the Alzheimer’s Society UK, smoking may increase your risk of developing dementia and Alzheimer’s. There is also evidence that quitting may reduce your risk.
Here are some tips to quit smoking from the National Institute on Aging:
-
Seek help from a healthcare provider
-
Enroll in group or individual counseling
-
Start a new activity to take your mind off of smoking
-
Get a prescription for medications that may help with symptoms of nicotine withdrawal
Stay connected
Socializing is believed to cut the risk of dementia. Socializing with family, friends and neighbors may reduce the risk of depression and possibly delay the onset of dementia.
It is also important to stay mentally active. Participating in mentally challenging activities, such as learning a new skill or new topic, may support brain health and help stave off dementia. Things like board games, crafts or volunteering may help keep your brain stimulated and connected.
Sleep well
Sleep is important for your mind and your body. Aim for ۸ hours of sleep a night. If you are sleeping poorly, talk to your healthcare provider about possible remedies.
Hear it all
Older adults with hearing loss may have trouble interacting with others. Avoid loud sounds to prevent hearing loss, and see an audiologist if you believe you might need hearing aids.
Watch your head
Wear a helmet when bicycling. Wear sturdy shoes when walking. Wear a seatbelt when riding in a car. It’s important to protect your head from concussions and brain injuries that may lead to dementia and Alzheimer’s.
Living with Alzheimer’s
It’s important that people who are diagnosed with Alzheimer’s receive regular medical care. They should see their primary care doctor, as well as specialists, such as a neurologist, neuropsychiatrist or geriatric psychiatrist, as needed.
Finding and signing up for a memory disorders clinic might be helpful to some patients and their families.